What is Gum disease?
Gum disease, or periodontitis, is a very common condition that affects the structures that surround and support your teeth such as the gum and bone. Most adults in the UK have it to some extent, and it is in fact the sixth most prevalent disease worldwide.
Despite being so widespread, it can often go unnoticed for many years, and if left undiagnosed and untreated, it can go onto leading to tooth loss in a group of people.
What causes Gum disease?
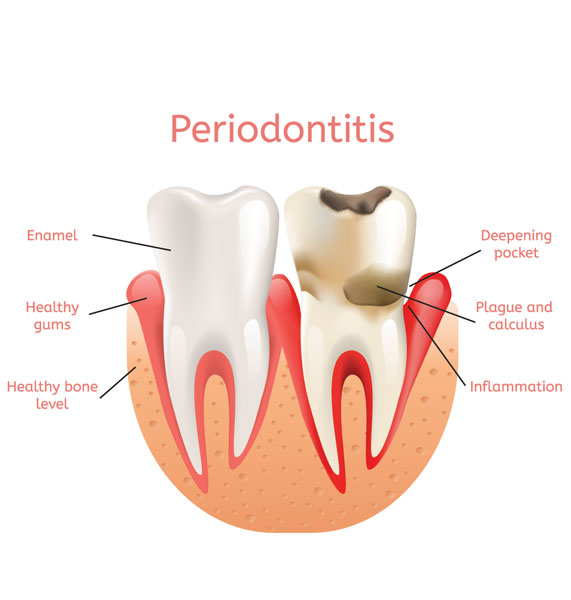
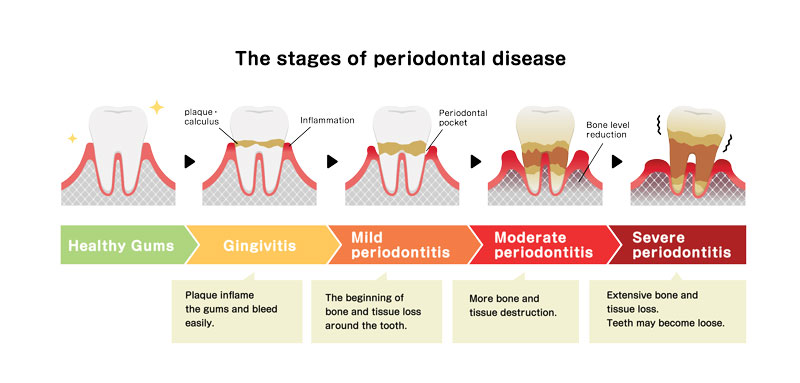
Gum disease is caused by a build-up of bacteria on tooth surfaces, which accumulate over time to form a sticky substance known as plaque. As plaque accumulates on teeth, it may lead to your gums becoming swollen, red and inflamed and may start to bleed/become sore. This early stage of gum disease is known as gingivitis. In some people if left untreated, this may progress to a more advanced form of gum disease, known as periodontitis, where the gums and bone surrounding the teeth are progressively destroyed, leading them to separate and lose their attachment to the teeth. Eventually this may lead to loosening and mobility of the teeth, causing them to fall out.
What is a Periodontist?
A periodontist is a dentist with additional specialist training in the prevention, diagnosis, and treatment of gum (or periodontal) disease. While gum disease can be managed in some by their general dental practitioner, a specialist periodontist is equipped with experience and the latest techniques in managing more advanced disease.
At the first appointment, your periodontist will review your overall medical and dental health and may then proceed to evaluate the health of the gums, making exact measurements to note the most affected sites and take X-rays to establish the condition of the underlying bone.
Based on this assessment, the periodontist will plan your treatment accordingly in order to effectively manage and control the disease as necessary.

Who is likely to get gum disease?
While all gum disease is caused by plaque, certain groups of people may be more susceptible to developing more advanced forms of gums disease (approximately 10% of the population). These include:
- People with a family history of gum disease
- Smokers
- People with poorly controlled diabetes
- People taking certain medications, such as some drugs that help control high blood pressure or epilepsy.
- Lifestyle factors such as stress
- Certain general diseases
Recognising the signs of gum disease
The signs of gum disease may vary greatly, however some general signs may include bleeding gums when brushing or eating, swollen or red appearance of the gums, drifting/tilting or wobbly/loose teeth, changes in the way you bite your teeth together, bad breath and receding gums.
It is important for you to see a dentist if you believe to have any of the signs of gum disease so it can be investigated, diagnosed and managed in a timely manner
Preventing Gum Disease
Gum disease can be prevented or controlled. The most important advice in preventing the progression of gum disease is maintaining effective oral hygiene to remove accumulating plaque from all tooth surfaces on a daily basis. Good toothbrushing technique and cleaning in between the teeth using interdental brushes and/or floss is key to this. Maintaining regular dental appointments and hygiene visits may also allow a dental care professional to spot the signs of gum disease, give specific tailored advice and any necessary treatment to help stop the progression of the disease.

Periodontal treatment – treatments available to control gum disease
Based on the extent of gum disease, your periodontist may suggest one or a combination of the following treatments as part of an overall management plan:
- Specific oral health education and advice: as plaque is the primary cause of all gum disease, it is important to be able to remove plaque effectively at home, and as such your periodontist will explain thoroughly the best cleaning aids specific to your mouth and how to best use them.
- Professional cleaning: specific cleaning instruments can be used by your practitioner to remove all soft plaque deposits on the accessible parts of your teeth followed by the harder deposits such as calculus which build-up in inaccessible areas such as the pockets surrounding your teeth. All exposed tooth surfaces will then be treated with Fluoride to help prevent sensitivity.
- Antibiotic therapy: in some cases, where the gum disease has not responded to conventional oral hygiene measures, your practitioner may prescribe a course of antibiotic therapy to manage persistent gum infection alongside other treatment.
- Surgical periodontal treatment: in some cases, a minor surgical procedure may be required to expose tooth root surfaces under the gum line in order to clean them more effectively. This involves lifting the gum away from the tooth surface under local anaesthetic, thoroughly cleaning all surfaces removing plaque and bacteria, and then stitching the gum back in place. Sometimes your periodontist may even suggest regenerative periodontal therapy, where areas of bone loss can be treated if suitable. Periodontists are also qualified to use surgical techniques to treat gummy smiles and to improve or correct areas where the gums have receded.
- Reassessment: for any patient suffering from gum disease, review and reassessment is of paramount importance after each course of treatment to ensure that disease does not progress or recur.
